The retina is an integral part of the overall structure of the eye, since this light-sensing membrane is involved in capturing and transmitting images to the brain. Small holes or tears in the retina wall can lead to retinal detachments. It is important to treat retinal detachments effectively and quickly, because the shrinking of the eye's vitreous gel or the thinning of the retina can even lead to vision loss. This is fairly common in middle-aged individuals and older people, and people who are nearsighted or have a genetic predisposition.
When Should a Detached Retina Surgery Be Taken?
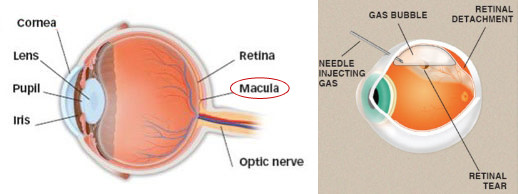
To prevent vision loss, it is imperative to treat retinal detachments in order. Ideally, the surgery should be performed on the same day if the central vision area, also known as the macula, is not affected by the detachment. This will prevent any further detachment and also increase the chances of maintaining good vision.
In case of macula detachment, it is difficult to restore vision to normal, but detached retina surgery may be performed to avoid total blindness. And your eye doctor will arrange your surgery after waiting 7 to 10 days.
Detached Retina Surgery Procedures
There are different surgical procedures for retinal detachment treatment. A laser treatment or cryotherapy (freezing) is enough to treat a simple retinal tear. Cryotherapy is also used to treat tears during other serious surgeries.The type of surgery and anesthesia should depend on the type of retinal detachment.
Pneumatic Retinopexy
In pneumatic retinopexy, the doctor injects a gas bubble into the eye, which gently presses the retina back into its place. Cryotherapy probe or laser beam then reattaches the retina into place, and the bubble inserted gradually dissolves over a couple of days. This procedure can be carried out at the doctor's office.
Scleral Buckle Procedure
A flexible band may be placed around the eye in order to counter the force that makes the retina out of its place. This is known as a scleral buckle procedure. It drains any fluid behind the detachment, so that the retina is able to come back to its place. This procedure is used for serious cases and has to be carried out in a surgery or hospital. It involves the administration of general or local anesthesia, but the patient does not necessarily have to stay overnight on a clinic or hospital.
Vitrectomy
Another procedure used for serious cases is vitrectomy. This involves the partial removal of the vitreous fluid of the eye. This procedure can empower the doctor to better access to the retina and tissues around. Your doctor can flatten the retinal detachment directly, peel off the scar tissue of retina, and fix holes or reattach apparent large tears. This procedure has to be carried out in a surgical clinic and involves local anesthesia.
Are There Any Risks of Detached Retina Surgery?
Although it is rare, there are several risks involved in detachment surgery just like many other surgeries, and you may not get your full vision restored.
Bleeding, infections (like endophthalmitis) and increased eye pressure (also known as elevated intraocular pressure) are common risks of a detached retina surgery. You may also experience another detachment on retina after the surgery. Since anesthesia is given to patients, they may have problems in breathing and may react to the medicines.
Another complication is proliferative vitreoretinopathy, which leads to contractions and scarring on the retina after repair, and further surgery may be needed to treat this conditions. The risk of developing complications increases in patients who have glaucoma, cataracts, poor overall health and a high degree of retinal damage.
What to Expect After Detached Retina Surgery
1. Vision Improvement
It may take up to a couple of months for the patient's vision to improve. It may never be fully restored. Those suffering from chronic retinal detachment may not recover their vision. In general, the longer a detachment has been present for and the severer it is, the less chancesof vision recovery are.
2. Eye Patch
After a retinal detachment repair surgery, most patients can expect to suffer from a certain level of discomfort. Typically, the ophthalmologist asks the patient to cover the eye with an eye patch or shield. This is usually not to be taken off until the first follow up visit, which usually takes places the next day. During this visit, the doctor will remove the eye patch.
3. Medications and Eye Drops
Any medications needed by the patient are also prescribed by the doctor. During the first follow up visit with the doctor, he will prescribe any eye drops that are needed with proper dosage. Generally, patients are not required to use any special eye drops the very night after the surgery. They are also asked to bring any eye drops that they have been using to the first consultation with the doctor after the surgery. In case of pain, patients are advised to take Tylenol (also known as acetaminophen). Ibuprofen and aspirin should be avoided since they can increase the risk of bleeding.
4. Special Tips After Gas Bubble Insertion
If a patient has undergone a procedure that involved the insertion of a gas bubble, he or she may be asked to keep their head in a special position for a while, which is discussed with the patient and the family right after the surgery. The position recommended by the doctor depends on where the patient's retinal tear is. It is imperative to adhere to the instructions given by the doctor, since a failure to do so can lead to detaching. Besides, a procedure involving gas bubble usage requires the patient to avoid air travel, going under anesthesia and scuba diving. Some patients may also have to get their glasses changed.
When to Seek Medical Attention
Patients themselves should also monitor the recovery very well, and immediately get in touch with your doctor in case of problems like coughs, new or worse symptoms, any sign of infection, chills and fever, changes in vision, increase in pain, discharge, bleeding, swelling or redness of the eye.
