One of the most important vitamins for our body is vitamin D and more is continually learned about its functions. Nearly every cell and tissue has vitamin D receptors, making it vital to the health of the entire body. Vitamin D deficiency could lead to many illnesses such as cancer, heart disease, and hypothyroidism. Vitamin D and thyroid functions are closely intertwined.
What to Know About Vitamin D

Vitamin D isn’t actually a vitamin—it’s really a fat-soluble steroid hormone precursor. It’s primarily obtained from exposure of the skin to the sun, or from a few foods such as cod liver oil, sardines, salmon, and eggs. But we get vitamin D mainly from milk and orange juice, and other foods that are fortified with vitamin D.
2 different compounds make up vitamin D: ergocalciferol, which is vitamin D2 and is found mainly in plants, and cholecalciferol, vitamin D3, mainly found in animals. Both components together are simply referred to as vitamin D.
What’s the Function of Thyroid Gland?
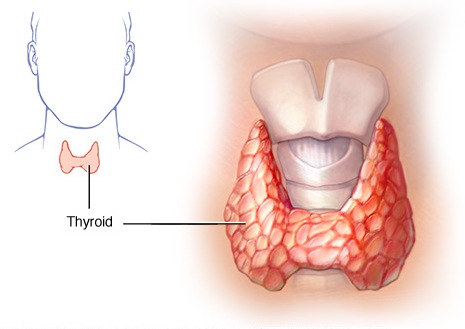
The largest gland in the neck is the thyroid gland, and it is shaped somewhat like a butterfly. It is on the front side of the neck underneath the skin and muscle tissue. The left and right “butterfly wings” are the left and right thyroid lobes that wrap around the trachea. The only function of the thyroid is to produce the thyroid hormone, which takes on a number of different forms including T3 and T4, and is vital to all parts of the body. It increases cellular function and regulates the metabolism. The thyroid hormone is produced from iodine, and is controlled by the thyroid stimulating hormone (TSH) which is released by the pituitary gland. The TSH is used as an indicator of thyroid function.
How Are Vitamin D and Thyroid Diseases Related?
In order to understand how vitamin D and thyroid work together, you must first have a basic grasp of how vitamin D works inside the body. Once ingested, vitamin D travels to the liver. There it’s converted to calcidiol, but calcidiol is only a prohormone. So it’s converted to calcitriol, which is the bioactive form of the vitamin. The conversion process takes place in the kidneys, or in the macrophages and monocytes of your immune system.
When the calcitriol has been released into your bloodstream, it binds to a plasma carrier protein. This protein is the taxi that carries vitamin D around your body to the various sites of action. Now, for vitamin D to act, it must bind to the vitamin D receptors that are found in nearly all of the body’s organs. The vitamin D found with these receptors is of great importance to the thyroid gland.
It is now known that people with hypothyroidism also have low levels of vitamin D. This condition is thought to be caused by one of two following issues:
1. Poor absorption of vitamin D from the intestine,
2. Your body isn’t activating the vitamin properly.
How Much Vitamin D Should I Take to Treat Thyroid Disorders?
There is no standard formula for treating vitamin D deficiency in people with thyroid disorders. You should never self-treat, but should be under the close supervision of your physician, with regular monitoring and testing of vitamin D levels.
There is no firm consensus on the dosage of vitamin D used for treatment. Recommendations range widely from 10,000 IU all the way down to 2,000 IU. Part of this fluctuation depends on how serious your deficiency is, and that can vary during the span of treatment. The standard norm for healthy people is 20-50ng/mL of vitamin D. But when treating people with autoimmune thyroid disorders, a much higher value should be aimed at. This is because the higher levels of vitamin D are needed in order to stimulate the normal responses from polymorphic Vitamin D receptors in people with autoimmune disorders.
When it comes to vitamin D and thyroid disorders, basic recommendations begin with 6,000 IUs daily if your tested levels of vitamin D are below the normal values. If you’re closer to the lower end of the normal range, 4,000 IUs may be sufficient. To maintain good levels, a dose of 2,000 IUs daily should work. When taking the higher doses of vitamin D, watch your calcium levels. Hypercalcemia is a major indicator of vitamin D toxicity. Make certain that your calcium levels are kept below 110,000ng/mL at all times during treatment.
Clinical Treatment Suggestions
When I’m treating a patient for vitamin D and thyroid related deficiency, I very cautiously raise the serum level up, providing a range between 0.06-0.07ng/mL. When the symptoms get better at this level, I switch to maintain levels, watching carefully for signs of toxicity, which include nausea, vomiting, nervousness, weakness, excessive thirst and urination, poor appetite, and kidney stones.
Because calcium that’s elevated in the blood is an indicator of vitamin D toxicity, and a serious cardiovascular disease risk factor, I also monitor the serum calcium levels, making certain that they don’t go over 110,000-120,000 ng/mL.
I also see to it that my patients get the right amounts of vitamins A and K2. You can find vitamin A in whole milk, leafy green vegetables, eggs, orange and yellow vegetables, fruits, tomatoes, and some vegetable oils. Vitamin K2 is found in fermented foods such as natto and kefir, but also in hard and soft cheeses, egg yolk, and butter from grass-fed cows. I sometimes use a K2 supplement for patients who can’t stomach fermented foods.
Lastly, let’s also look at the treatment experiences from some patients: